Background: Extending implantable cardioverter defibrillator (ICD) detection windows improves outcomes by reducing unnecessary therapies; a 1% reduction in therapies results in ~1% reduction in mortality. However, waiting too long for episodes to self-terminate may prolong cardiac ischaemia, which could compromise the effectiveness of ICD treatments. We have previously shown that laser Doppler perfusion monitoring, combined with an electro-mechanical coupling algorithm to reduce the impact of noise (SafeShock), can be used to assess peripheral perfusion. This method allows reliable detection of haemodynamic compromise during ventricular fibrillation. However, the impact of ventricular tachycardia (VT) on central and peripheral haemodynamics and its potential application to ICD therapies has not been previously studied. We assessed coronary blood flow (CBF), central pressure and peripheral perfusion (PP) during simulated VT.
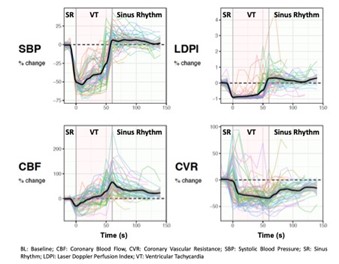
Methods: In patients having a coronary angiogram, we simulated VT by pacing the right ventricle at rates of 180 and 200 bpm. We recorded continuous ECG, invasive CBF and central aortic blood pressure (cAoBP), and non-invasive peripheral laser Doppler perfusion. Coronary vascular resistance (CVR) was calculated by dividing CBF by the mean aortic pressure. We assessed the haemodynamic impact during the first 30 s and second 30 s (30–60 s) of VT, relative to baseline. Laser Doppler data was analysed using the SafeShock algorithm. We used a cut-off of 5.2 au to assess its ability to discriminate severe haemodynamic compromise during VT (defined by a reduction in cAoBP ≥-35%) from those without.
Results: We simulated 61 VT episodes in 19 patients (mean age 64, left ventricular ejection fraction ≤40% in 6 patients [32%]). We observed a mean reduction in CBF during the first 30 s of VT (-15%, p<0.0001), but in the next 30 s, mean flow increased above baseline (+ 12.5%, p=0.002). CVR reduced during the 30–60 s window (-12.6%, p<0.0001), possibly aiding autoregulation of CBF. cAoBP and PP also decreased in the first 30 s of VT, but by a greater magnitude than CBF: -50.7% cAoBP, -91% PP (both p<0.0001). However, in contrast to CBF, both cAoBP (-39%) and PP (-85%) remained below baseline after 30 s of VT. Haemodynamic responses during VT episodes varied. In the first 30 s of VT, CBF was preserved in 29.5% of VT episodes, whereas by 30–60 s, flow recovered in 75.4%. We observed a <35% reduction in cAoBP and PP in 6.6% and 0% of VT episodes, respectively, in the first 30 s, and in 37.5% and 0% in the next 30 s. We investigated the utility of using peripheral Laser Doppler perfusion measurements to differentiate between VT with and without severe haemodynamic compromise. Using a threshold of >5 au (which is independent of baseline measurements) as the threshold for withholding ICD therapies, provided an 11% reduction in ICD therapies, and did not result in therapies being withheld during episodes with severe haemodynamic compromise or a fall in CBF (sensitivity 100%, specificity 33.3%).
Conclusion: Coronary blood flow was preferentially protected during VT and preserved in over 2/3 of VT episodes with rates of 180 and 200 bpm. This suggests these ICD therapies could be safely withheld without prolonging cardiac ischaemia. Utilising a haemodynamic sensor could reduce unnecessary therapies by identifying VT episodes without severe haemodynamic compromise. ❑
Figure 1