Introduction: Current guidelines indicate that pacing methods that maintain physiologic ventricular activation (biventricular pacing or His-bundle pacing) should be chosen over right ventricular pacing among patients with EF 36-50% who are expected to require ventricular pacing >40% of the time. There are no guidelines to help predict which patients will receive a high burden of ventricular pacing and this is left to operator opinion. We sought to ascertain whether operator opinion is an accurate predictor of high burden of ventricular pacing.
Methods: This was a single-centre single-blinded observational study of patients who received pacemaker implant for treatment of bradycardia over the 4-year period to the end of April 2019 and had at least 12-month follow-up data on record. Patients’ demographic, clinical, electrocardiographic and echocardiographic data were reviewed in a blinded fashion by a senior implanting physician, who estimated whether the percentage right ventricle pacing at 12 months would exceed 40%. At 12 months the percentage of pacing was then identified from the pacing records and compared with the prediction.
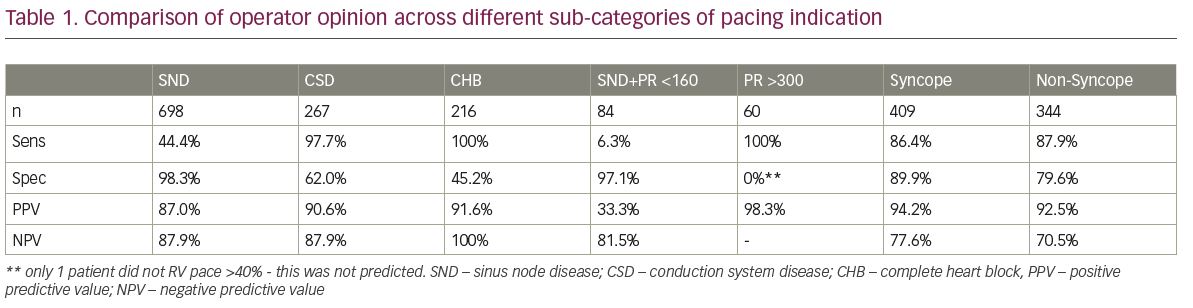
Results: Some 982 patients underwent pacemaker implantation during the study period, 698 for conduction system disease (CSD), 267 for sinus node disease (SND) and 17 for other conditions. Overall, 856 had valid follow-up data. Of these, 543 (63.4%) were predicted to ventricular pace >40% of the time and 527(61.6%) were documented as actually having paced >40%. The sensitivity and specificity of operator prediction were 93.2% and 84.2% respectively, with positive and negative predictive values of 90.4% and 88.5%. Table 1 illustrates the above analysis and further sub-group analysis of different populations by clinical parameter. In the sub-group analysis, clinical heart block and PR>300 conferred a significant predictive factor for accurate prediction of >40% RV pacing, but that clinical features such as syncope or non-syncope were
less useful
Conclusion: In this single-centre study, in patients receiving pacemaker implant for treatment of bradycardia, operator prediction of the burden of RV pacing >40% has an acceptable degree of accuracy. Patients with sinus node disease ventricular pacing more than 40%, and those with conduction disease ventricular pacing less than 40% were harder to pick up. Sub-group analysis alludes to the fact that certain clinical parameters may make this prediction easier. Assessing for easily obtainable clinical, electrocardiographic or echocardiographic parameters to such an end, may lead to greater accuracy of prediction.