Aims: Previous studies have evaluated the incidence and prognostic significance of syncope in ICD recipients; however, these have been almost exclusively derived from randomised controlled trials (RCTs) of primary prevention patients with severe left ventricular systolic dysfunction (LVSD). There is little evidence of the impact of syncope in implantable cardioverter defibrillator (ICD) patients in a real-world setting. This single-centre retrospective study sought to evaluate the incidence and prognostic significance of syncope in an unselected population of ICD patients including patients with secondary prevention and less severe LVSD.
Methods: Data were collected on consecutive patients undergoing first ICD implantation between January 2009 and December 2019. The primary endpoints were first occurrence of all-cause syncope, all-cause mortality and all-cause hospitalisation. Multivariate Cox proportional hazard models were used to identify risk factors associated with syncope and to analyse the subsequent risk of mortality and hospitalisation.
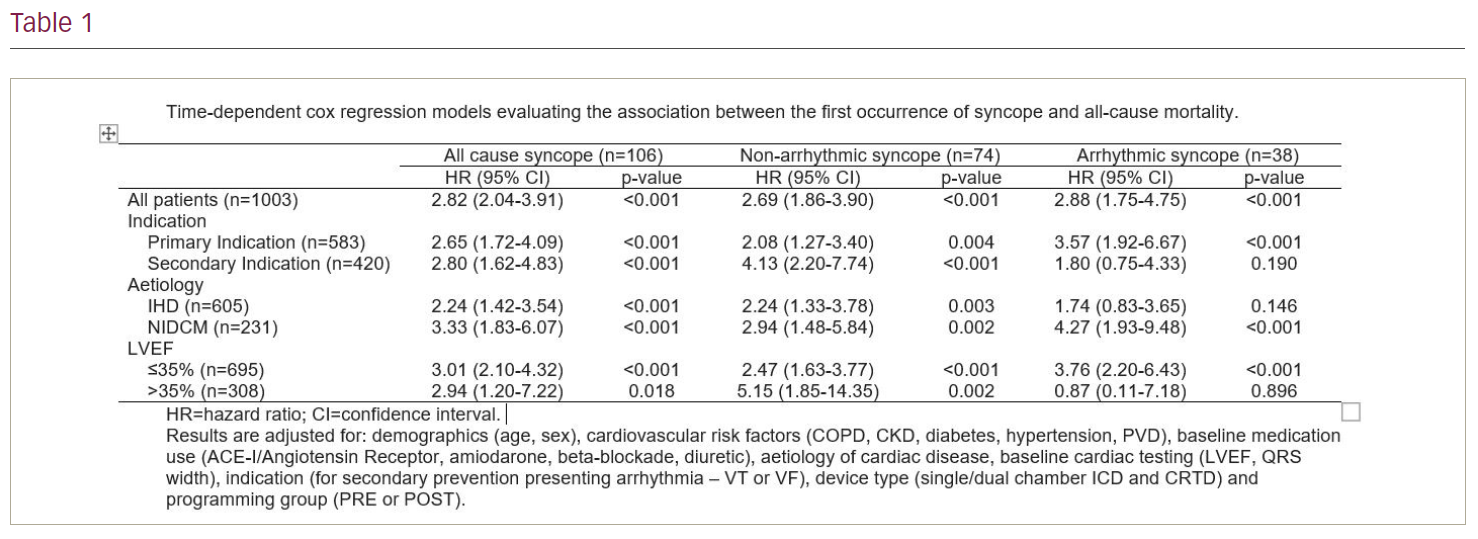
Results: A total of 1003 patients (58% primary prevention) were included in the final analysis. During a mean follow-up of 1,519 ± 1,055 days, 106 (10.6%) experienced syncope, 304 died (30.3%) and 477 (47.5%) were hospitalised for any cause; 106 (10.6%) patients experienced all-cause syncope, 38 (3.7%) arrhythmic syncope and 74 (7.4%) non-arrhythmic syncope, including six patients (0.6%) with both arrhythmic and non-arrhythmic syncope. The 1-, 3- and 5-year all-cause syncope rates were 3.8%, 8.3% and 13.3%, respectively. The arrhythmias associated with arrhythmic syncope were VT (n=23, 60.5%), VF (n=11, 28.9%) and atrial arrhythmias (n=4, 10.5%). In an analysis adjusted for baseline variables, the first occurrence of syncope was associated with a significantly increased risk of mortality (HR 2.82, p<0.001) and first occurrence of hospitalisation (HR 2.46, p=0.002).
Conclusion: There were three main findings from this study. First, syncope, irrespective of the cause, portends a poor prognosis with significant associations with both mortality and hospitalisation. In multivariable analyses the first occurrence of all-cause syncope, arrhythmogenic syncope and non-arrhythmogenic syncope were all associated with a significant increase in mortality and hospitalisation. Second, the relationship between all-cause syncope and mortality remained significant in secondary prevention patients and in patients with less severe LVSD (LVEF >35%). Third, in multivariable analysis, strategic ICD programming, with long detection times and high detection zones, was not independently associated with an increase in first occurrence of syncope. ❑