Introduction: Multiple independent investigations have demonstrated heterogeneity in radiofrequency (RF) effects during pulmonary vein isolation (PVI) in humans, with all data indicating significantly greater RF effects at the left side of the left atrial posterior wall (LAPW). Mechanisms underlying these findings have yet to be determined, however investigations of immediate pre-ablation impedance as an indication of catheter-tissue contact surface area (CCSA), under different ventilatory conditions, may provide insights.
Methods: Single operator contact force (CF) and VISITAG Module-guided PVI was performed in a standardised fashion in consecutive, unselected adults with symptomatic AF: temperature-controlled RF, 17 ml/min; CF filter 100% minimum 1 g; position stability 2 mm; ACCURESP ‘off’; atrial overdrive pacing at 600 ms; Agilis sheath. Initially, PVI was performed during volume-controlled intermittent positive pressure ventilation (IPPV) at 30 W (n=23); a second cohort comprised high frequency jet ventilation (HFJV) at 20 W to left-sided LAPW sites and 30 W elsewhere (n=11). Annotated data at ablation naive, first sites of LAPW RF delivery (protocol target RF duration 15 s) were retrospectively analysed following export. Minimum impedance from ’AblationData’ files was subtracted from impedance at RF onset (i.e. ‘Base impedance’, BI), to derive ‘∆Base impedance’ (∆BI).
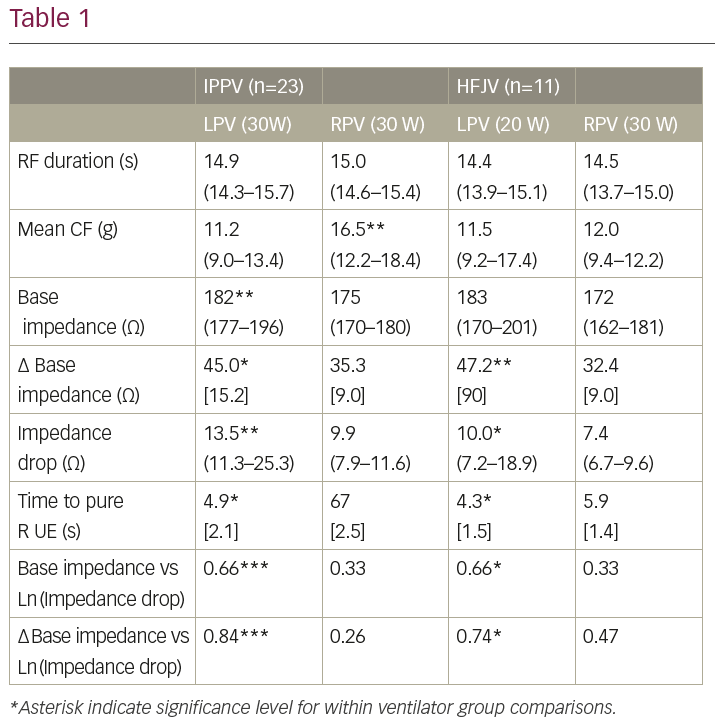
Results: RF effects judged by impedance drop (ID) and time to pure R unipolar electrogram (UE) morphology change were significantly greater at left versus right-sided LAPW first-ablated sites (Table 1; mean [SD] or median (first to third quartiles), as appropriate). In the IPPV cohort these findings occurred despite significantly greater mean CF at right-sided sites (16.5 g versus 11.2 g, p=0.002), and in the HFJV cohort despite “per-protocol” 33% lower RF power delivery at left-sided sites. The IPPV cohort demonstrated significantly higher BI at left versus right-sided sites (182 Ω versus 175 Ω, p=0.002), while both cohorts demonstrated significantly greater ∆BI at left-sided sites (IPPV 45Ω versus 35 Ω, p=0.01; HFJV 47 Ω versus 32 Ω, p=0.001). For IPPV and HFJV cohorts and at left-sided sites, BI and ∆BI demonstrated significant positive correlation with RF effect (i.e. Ln(ID)), strongest with ∆BI (IPPV r=0.84, p<0.0001; HFJV r=0.74, p=0.01). In contrast, at right-sided sites the IPPV cohort demonstrated no significant correlation between either BI/∆BI and Ln(ID), while the HFJV cohort demonstrated weak positive correlation between ∆BI and Ln(ID), not reaching statistical significance.
Conclusions: Significantly greater CCSA mediates greater RF effect at left versus right-sided LAPW sites in vivo. Furthermore, the absence of correlation between CCSA and RF effect at right-sided sites indicates important out-of-phase catheter-tissue interaction, not eliminated by HFJV. These mechanistic insights may help improve the efficacy and safety of RF delivery during PVI.