Introduction: Catheter ablation is the treatment of choice for accessory pathways (APs). Currently, it is unclear whether the use of electro-anatomical mapping (EAM) systems results in better outcomes of radiofrequency (RF) AP ablations. To help answer this question we present a retrospective observational analysis of a modern single centre cohort.
Methods: Clinical and electrophysiological data were extracted from patient records for all AP ablations performed in our centre between May 2018 and December 2019. Outcome data were compared between EAM and non-EAM cases. Continuous variables are given as median [interquartile range]. Group comparisons were performed using the Mann-Whitney U test (continuous variables) or Fisher’s exact test (categorical variables).
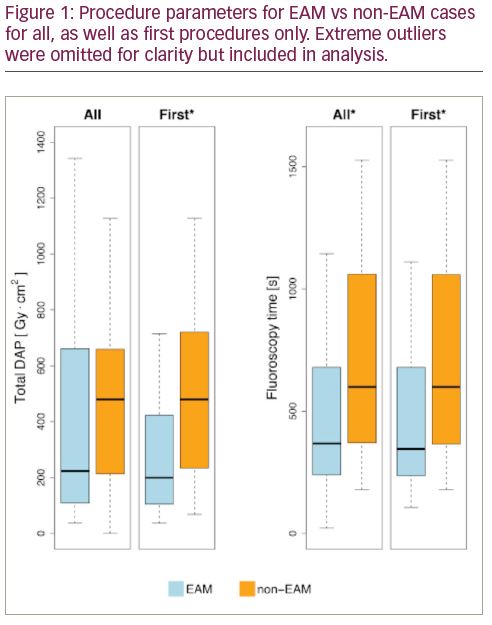
Results: A total of 82 patients underwent 85 RF ablation procedures (66 first and 19 repeat). EAM was used in 57 cases while 28 were in the non-EAM group. The median age was 35 [26–47], 27 patients were female, 5 had congenital heart disease, 15 had co-existing atrial fibrillation, 38 had a documented tachyarrhythmia, and 58 had manifest pre-excitation on ECG. The presenting symptoms were palpitations in 69 patients, syncope in 6, cardiac arrest in 2, others in 4, and 4 cases were diagnosed incidentally. Pathway location was left in 41, right in 11, and septal in 33. The success rate was 95% (81/85) acutely, and 91% (77/85) at 3 months. The re-do rate was 7% (6/85), and the overall significant complication rate was 4% (3/85): 1 tamponade, 1 myocardial infarction, and 1 vascular access complication (haematoma not requiring any intervention). There were no statistically significant differences in terms of these outcomes between EAM and non-EAM cases. Fluoroscopy time was shorter in EAM cases (368.0 s [239.0–680.0] vs 599.0 s [371.0–1060.5], p<0.01), but the difference in dose area product (DAP) did not reach statistical significance (223.1 Gy·cm2 [109.2–646.9] vs 479.7 Gy·cm2 [213.0–659.3], p=0.15). Procedure time was longer in EAM cases (158.0 min [126.0–180.0] vs 123.0 min [112.5–147.5], p<0.01). Among first procedures there was a statistically significant difference in fluoroscopy time (345.5 s [236.2–663.8] vs 599.0 s [366.0–1059.0], p<0.01) and DAP (199.3 Gy·cm2 [105.1–423.0] vs 479.7 Gy·cm2 [233.1–720.6], p=0.02) and no significant difference in procedure time (144.0 min [121.5–168.5] vs 123.0 min [112.0–146.0], p=0.06) in EAM vs non-EAM cases respectively.
Conclusions: EAM use correlates with reduced radiation exposure in patients undergoing AP ablation with at most a modest increase in procedure time and no difference in clinical outcomes. The reduction is particularly pronounced in first procedures. This finding provides an argument for more liberal use of EAM, as well as a rationale for further research.