Catheter ablation (CA) is an invasive adjunctive therapeutic option for atrial and ventricular arrhythmias, in uncontrolled cases, following optimal medical therapy.1,2 The validation of 3D mapping and its implementation into clinical usage has been a remarkable achievement in the field of complex ablation of scar-related ventricular tachycardia (VT) in the early 2000s.3 In the setting of atrial fibrillation (AF), 3D navigation systems have been crucial for reducing complications, including pulmonary vein (PV) stenosis, perforation, phrenic nerve or oesophageal injury, during pulmonary vein isolation (PVI), or substrate modification, defragmentation or linear ablations, during chronic AF ablation.4–6
While clinical characteristics and the operators’ experience can affect long-term success rates of CA, the acute success rate is less dependent on clinical variables during the follow-up period, and therefore, it is a better marker of the efficacy of the different mapping systems.7–9 This systematic review aims to summarize the existing data about the acute arrhythmia termination success rates in atrial and ventricular CA procedures using the most common mapping systems (CARTO [Biosense Webster Inc., Diamond Bar, CA, USA], Rhythmia [Boston Scientific, Natick, MA, USA], CardioInsight [Medtronic Inc, Minneapolis, USA] and NavX/EnSite [St. Jude Medical, St Paul, Minnesota, USA]).
Materials and methods
This systematic review was performed in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses statement.10
Search strategy
This study aimed to identify all relevant studies that provided data about the acute success rates of different mapping systems in patients who underwent the CA procedure either for AF and atrial tachycardia (AT) or for VT and premature ventricular contractions (PVCs). Two independent investigators performed a systematic search in MEDLINE and Cochrane databases through July 2021. The reference lists of the included studies, as well as relevant review studies, were manually searched. The following keywords were used to retrieve all relevant studies: “(CARTO OR Rhythmia OR NavX OR CardioInsight OR EnSite) AND (atrial OR ventricular) AND (fibrillation OR tachycardia OR flutter)”, without any limitations. We first screened the titles and abstracts of each retrieved study, and if a study was considered relevant, then the full text was studied.
Inclusion/exclusion criteria
We included studies that provided data on acute success rates during ablation procedures in either AF/AT or VT/PVCs across the different mapping systems. Acute success is defined either as clinical arrhythmia termination or as any arrhythmia termination or non-inducibility. The definitions of arrhythmia termination that were used in each study are presented in Tables 1 and 2.
Table 1: Baseline characteristics and main outcomes of the included studies related to atrial arrhythmia catheter ablation procedures
|
Study (year) |
Country |
Single/multicentre |
N |
Type of arrhythmia |
Mean age (years) |
Males (%) |
EF (%) |
Mapping system |
Acute success, N (%) |
Acute success definition |
Mapping technique |
Catheter type |
Complications |
Follow-up (months) |
Recurrence at the f/u (%) |
Fluoroscopy time (min) mean ± SD |
|
Atrial arrhythmias |
||||||||||||||||
|
CARTO mapping system |
||||||||||||||||
|
Calvo et al. (2017)11 |
Spain |
Single |
13 |
Pers AF (long standing) |
53.9 |
100 |
57.7 |
CARTO |
2 (15.4) |
SR restoration |
Phase/frequency mapping |
Irrigated NaviStar ThermoCool SmartTouch, PentaRay and a quadripolar catheter (Biosense Webster) |
No complications |
12–72 |
30 |
17.7±3.9 |
|
Choo et al. 2011*12 |
UK |
Single |
47 |
PAF and Pers AF |
56.2 |
68 |
58.9 |
CARTO |
45 (96) |
SR restoration |
– |
Irrigated (Celsius or NaviStar ThermoCool [Biosense Webster] or Cool Path Duo [St. Jude Medical, St. Paul, MN, USA]) |
Cardiac tamponade (n=1) |
12 |
60 |
73±27 |
|
Nademanee et al. (2004)13 |
Thailand |
Single |
121 |
PAF and Perm AF |
63 |
76 |
n/a |
CARTO |
115 (95) |
Complete elimination of the areas with CFAEs or conversion of AF into normal SR for patients with both CAF and PAF |
Voltage maps |
Standard 4 mm tip catheter |
Cerebrovascular accident (n=1), cardiac tamponade (n=2), complete atrioventricular block (n=1), transient severe pulmonary oedema (n=1) and femoral arterial atrioventricular fistula (n=1) |
12 |
9 |
14.7±4.8 |
|
Seitz et al. (2011)14§ |
EU |
Single |
22 |
NPAF: 86.4% |
56.6 |
82 |
44.7 |
CARTO (Biosense Webster, Diamond Bar, CA, USA) |
21 (95.5% |
AF termination defined as the conversion of AF into SR or regularization into stable AT |
CFAE LA map |
2–5–2 mm electrode spacing (Xtrem; ELA Medical, Le Plessis-Robinson, France), 3.5 mm irrigated-tip quadripolar ablation catheter (2–5–2 mm interelectrode spacing, ThermoCool; Biosense Webster) |
None |
12 |
18 |
39±15 |
|
Seitz et al. (2013)14§ |
EU |
Single |
32 |
NPAF: 90.6% |
60.4 |
75 |
52.6 |
CARTO (Biosense Webster) |
30 (93.7) |
AF termination defined as the conversion of AF into SR or regularization into stable AT |
CFAE LA map |
Decapolar catheter (2–5–2 mm electrode spacing, Xtrem; ELA Medical), 3.5 mm irrigated-tip quadripolar ablation catheter (2–5–2 mm inter-electrode spacing, ThermoCool [Biosense Webster] F or J curve) |
None |
12 |
15.6 |
31±17 |
|
Suleiman et al. (2007)†15 |
Israel |
Single |
13 |
AF |
49† |
59† |
n/a |
CARTO system (Biosence Webster, Johnson & Johnson, USA) |
12 (92) |
Termination to SR |
– |
– |
Transient cerebrovascular accident (n=1) |
33* refers to the total population |
38.5 |
10.3±6.9* refers to the total population |
|
Takahashi et al. (2018)16 |
Japan |
Single |
68 |
AF |
62 |
68 |
59 |
CARTO 3 (Biosense Webster) |
35 (51.5) |
Termination into SR |
Activation mapping |
NaviStar ThermoCool SF catheter (Biosense Webster) |
None |
17.3 |
42.7 |
n/a |
|
Wang et al. (2009)17 |
China |
Single |
111 |
Pers AF |
50.8 |
55.9 |
53.1 |
CARTO (Biosense Webster) |
SR → 30 (27) AT → 35 (31.5) |
Termination to SR or AT (both data are provided) |
Activation mapping and CFAE mapping |
Decapolar catheter (Biosense Webster), decapolar circular mapping catheter (Lasso; Biosense Webster) and saline-irrigated 3.5 mm catheter (ThermoCool NaviStar; Biosense Webster) |
Catheter entrapment in valve prosthesis without further complications (n=1) and major stroke (n=1) |
4.1 med |
46.9 |
24±15 |
|
Wnuk-Wojnar et al. (2005)18 |
Poland |
Single |
94 |
PAF: 63.8% |
54.3 |
64.9 |
58 |
CARTO (Johnson/Biosense Webster) |
65 (69.6) |
Termination to SR |
Disappearance of electrical potentials within ablation lines and consequently inability to induce and maintain AF |
n/a |
Stroke (n=1), PV thrombosis (n=1), HIT (n=2) and pericardial tamponade (n=2) |
12 med |
30 |
22.4 (11–41) |
|
Wu et al. (2008)19 |
EU |
Single |
10 |
Pers AF |
62.3 |
50 |
n/a |
CARTOXP (Biosense Webster) |
3 (30) |
Termination of AF and/or prolongation of AFCL |
CFAE mapping |
4-polar distally circular catheter (OrbiterPV; C.R. Bard), octapolar reference catheter (XPTTM; C.R. Bard Electrophysiology, Lowell, MA, USA), 4 mm irrigated tip catheter (NaviStar ThermoCool; Biosense Webster) |
n/a |
n/a |
n/a |
n/a |
|
Suleiman et al. (2007)15† |
Israel |
Single |
37 |
AFL |
49† |
59† |
n/a |
CARTO system (Biosence Webster, Johnson & Johnson) |
35 (95) |
Termination to SR |
– |
– |
None |
33* refers to the total population |
10.8 |
10.3±6.9* refers to the total population |
|
Esato et al. (2009)20 |
EU |
Single |
26 (12 CARTO, 14 NavX) |
Macro-reentrant AT |
59 |
76.9 |
56 |
CARTO (Biosense Webster, Inc.) or NavX (Endocardial Solutions, Inc., St. Paul, MN, USA) |
26 (100%) for both systems |
Tachycardia termination and non-inducibility |
Entrainment |
Irrigated, F-type irrigated-tip, NaviStar ThermoCool [Biosense Webster]; M-Curve IBI Therapy Cooled Path [St. Jude Medical]) |
No complications |
10.1 |
12 |
37±19 |
|
Jamil-Copley et al. (2013)21 |
UK |
Single |
10 |
AT |
57.7 |
70 |
n/a |
CARTO-XP system (Biosense Webster, Haifa, Israel) |
9 (90) |
Increase in TCL |
Ripple, activation and entrainment |
– |
n/a |
n/a |
n/a |
n/a |
|
Okumura et al. (2016)22 |
Japan |
Single |
6 |
AT |
67 |
33.3 |
n/a |
CARTO 3 system (Biosense Webster) |
6 (100) |
Termination of AT and no inducibility of AT after isoproterenol infusion |
Activation and entrainment |
7F 4 mm tip (NaviStar; Biosense Webster), 5F quadripolar catheter (5–5–5 mm, inquiry catheter; St. Jude Medical), 5F decapolar catheter (Fe-po; Fukuda Denshi Co., Ltd., Tokyo, Japan) and 7F steerable duodecapolar Halo catheter (inquiry catheter; St. Jude Medical) |
None |
11 |
0 |
n/a |
|
Suleiman et al. (2007)15† |
Israel |
Single |
20 |
AT |
49† |
59† |
n/a |
CARTO system (Biosence Webster, Johnson & Johnson) |
15/20 (75) |
Termination to SR |
– |
– |
None |
33* refers to the total population |
25 |
10.3±6.9* refers to the total population |
|
Strisciuglio et al. (2019)23 |
EU |
Single |
31 |
AT |
69 |
63 |
n/a |
CARTO |
SR →23 (66) AT → 12 (34) |
AT termination to SR or AT with different cycle lengths |
High-density activation mapping and entrainment mapping |
Multi-electrode mapping catheter (PentaRay; Biosense Webster Inc., Irvine, CA, USA) and an open-tip irrigated RF catheter (8F) with tip-integrated contact force sensor (ThermoCool SmartTouch; Biosense Webster Inc.) |
n/a |
n/a |
n/a |
n/a |
|
Vicera et al. (2020)24 |
Taiwan |
Single |
20 |
AT |
58.2 |
75 |
59.6 |
CARTO 3 system ConfiDENSE Module |
SR → 18 (69.2) Another AT → 7 (26.9) |
Termination or change to a different activation pattern with an associated change in cycle length and negative inducibility of clinical AT |
Activation mapping and coherent map |
Multielectrode mapping catheter (Lasso Nav or PentaRay Nav; Biosense Webster, Inc.) |
n/a |
13.7 |
25 |
n/a |
|
Wo et al. (2014)25 |
Taiwan |
Single |
15 |
AT |
49 |
66.7 |
62 |
CARTO (Biosense Webster) |
15 (100) |
Termination of MRAT and non-inducibility |
Entrainment mapping |
4 mm NaviStar catheter (irrigating or non-irrigating; Biosense Webster) |
n/a |
15 |
0 |
n/a |
|
Yagishita et al. (2019)26 |
Japan |
Single |
39 |
AT |
65 |
78 |
59 |
CARTO 3 ConfiDENSE Module (Biosense Webster) |
90 |
Termination to SR |
LAT, voltage and entrainment |
Mapping catheter (PentaRay Nav; Biosense Webster), 3.5 mm irrigation catheter (ThermoCool; Biosense Webster) |
n/a |
n/a |
n/a |
n/a |
|
Rhythmia mapping system |
||||||||||||||||
|
Kitamura et al. (2018)27 |
EU |
Two-centre |
8 |
Biatrial AT |
59.5 |
87.5 |
59.9 |
Rhythmia (Boston Scientific, Marlborough, MA, USA) |
8 (88.9) |
Termination of biatrial AT to SR or to another AT |
High-density activation map |
3.5 mm tip open-irrigated catheter (ThermoCool SF; Biosense Webster), decapolar catheter within the coronary sinus (Extreme, Sorin/Dynamic XT; Boston Scientific) |
n/a |
12.4 med |
12.5 |
n/a |
|
Yamashita et al. (2019)28 |
EU and Japan |
Multicentre |
26 |
Post-AF ablation AT |
63 |
69 |
57 |
Rhythmia (Boston Scientific) |
25 (96.2) |
Restoration of SR or a change in the AT by RF ablation of the PV gap |
Activation and entrainment |
64-pole mini-basket catheter (Orion; Boston Scientific), non-magnetic open-irrigated catheter (Celsius, ThermoCool; Biosense Webster, Inc.) |
n/a |
12 |
15 |
n/a |
|
Anter et al. (2016)29 |
US |
Multicentre |
20 |
Recurrent AT |
62 |
n/a |
n/a |
Rhythmia (Boston Scientific, Cambridge, MA, USA) |
18 (75) |
Termination to SR |
Activation, entrainment and pace |
Orion basket catheter (Boston Scientific), nonmagnetic open-irrigated catheter (Celsius, ThermoCool; Biosense Webster) |
None |
7.5 |
25 |
n/a |
|
De Simone et al. (2020)30 |
EU |
Single |
24 |
Re-entrant AT |
54 |
54.2 |
n/a |
Rhythmia (Boston Scientific, Inc.) |
96.2‡ |
Termination to SR |
Propagation map and entrainment |
64-pole mini-basket mapping catheter (IntellaMap Orion; Boston Scientific, Inc.) |
None |
18 |
12.5 |
n/a |
|
Laţcu et al. (2017)31 |
EU |
Single |
19 |
AT |
71 med |
68.4 |
62 med |
Rhythmia (Boston Scientific) |
29 (97) |
Termination into SR or another stable AT |
Activation maps |
Decapolar diagnostic catheter (Inquiry L, 2–5–2 mm spacing; Saint Jude Medical), F-type, 2–8–2 mm spacing (Biosense Webster) and an IntellaMap Orion mapping catheter |
None |
12 med |
16 |
18±10 |
|
Takigawa et al. (2017)32 |
EU |
Single |
57 |
AT |
61.9 |
82.5 |
54.3 |
Rhythmia (Boston Scientific, Natick, MA, USA) |
66/88 (75)‡ |
AT termination |
Activation and entrainment |
Orion multipolar basket catheter (Boston Scientific), 3.5 mm tip ablation catheter (ThermoCool SF catheter; Biosense Webster) |
n/a |
6 |
26.3 |
n/a |
|
Takigawa et al. (2018)33 |
EU |
Single |
41 |
Post-AF ablation AT |
65.7 |
70.7 |
52.6 |
Rhythmia system (Boston Scientific) |
80.6‡ |
AT termination |
Activation |
Orion multipolar basket catheter, 3.5 mm tip ablation catheter (ThermoCool SF; Biosense Webster) |
n/a |
12 |
45.2 |
n/a |
|
NavX–EnSite mapping systems |
||||||||||||||||
|
Aksu et al. (2020)34 |
Turkey and USA |
Single |
12 |
Pers AF |
53 |
83 |
48.5 |
EnSite Precision (Abbott Medical, Chicago, IL, USA) |
8 (66.7) |
SR restoration |
Fractionation and mapping |
3.5 mm tip ablation catheter (TactiCath™ or FlexAbility™; Abbott), 20-pole spiral double-loop catheter (Inquiry™, AFocus II™ [Abbott]; 1 mm length, 4 mm spacing, 20 mm fixed-loop diameter) |
n/a |
34 med |
25 |
n/a |
|
Miyamoto et al. (2009)35 |
Japan |
Single |
50 |
Pers AF: 20% |
61.2 |
74 |
n/a |
EnSite version 6.0J (St. Jude Medical) |
75.6 |
AF termination to SR during PVAI alone or additional RF ablation |
Voltage and activation maps |
8 mm tip ablation catheter |
n/a |
14 |
8% |
n/a |
|
Miyamoto et al. (2010)36 |
Japan |
Single |
20 |
Pers AF: 20% |
58 |
70 |
n/a |
EnSite version 6.0J (St. Jude Medical) |
14 (70) |
AF termination to SR |
CFAE ablation |
7F catheter with an 8 mm tip distal electrode (Fantasista; Japan Lifeline Co. Ltd., Tokyo, Japan) |
n/a |
n/a |
n/a |
n/a |
|
Yamaguchi et al. (2010)37 |
Japan |
Single |
65 |
PAF |
58 |
84.6 |
n/a |
EnSite array |
47/51 (92.2) |
AF termination to SR |
Activation map |
20-pole circular mapping catheter (Optima; St. Jude Medical) and deflectable 7F quadripolar, non-irrigated 8 mm tip electrode ablation catheter (Fantasista; Japan Lifeline) |
No complications |
23 |
16.9 |
n/a |
|
Ammar-Busch et al. (2018)38 |
EU |
Single |
16 |
Pers AF |
63 |
88 |
n/a |
NavX (St. Jude Medical), ECVUE™ (CardioInsight Technologies, Inc., Cleveland, OH, USA) |
12 (75) |
AF termination |
CFAE mapping |
14 bipoles Orbiter PV, C. R. Bard or 20 bipoles AFocus II™ [St. Jude Medical], irrigated tip catheter (Therapy™ Cool Flex™; St. Jude Medical) |
No complications |
n/a |
n/a |
n/a |
|
Kumagai et al. (2013)39 |
Japan |
Single |
50 |
PAF and Pers AF |
63.9 |
78 |
61 |
NavX system (NavX, with CFE software; St. Jude Medical Inc.) |
18 (36) |
Termination to SR |
CFAE, activation and mapping |
7 F decapolar circular catheter (Lasso; Biosense Webster, Inc) and 3.5 mm irrigated tip RF catheter (Safire; St. Jude Medical Inc.) |
n/a |
12 |
28 |
n/a |
|
Kumagai et al. (2017)40 |
Japan |
Single |
32 |
AF |
57 |
87.5 |
63 |
NavX system (NavX with CFE software; St. Jude Medical Inc.) |
26 (81.3) |
AF termination or >10% slowing of the AF cycle length from after the PVI to the end of the high-DF and continuous CFAE-site ablation |
CFAE, activation and mapping |
7F decapolar circular catheters (Lasso; Biosense Webster, Inc.), 3.5 mm irrigated tip radiofrequency catheter (Safire; St. Jude Medical Inc.) and a 20-pole mapping circular catheter (St. Jude Medical Inc.) |
No complications |
12 |
19 |
n/a |
|
Choo et al. (2011)*12 |
UK |
Single |
24 |
PAF and Pers AF |
62.2 |
71 |
55.4 |
NavX |
24 (100) |
SR restoration |
– |
Irrigated (Celsius or NaviStar ThermoCool [Biosense Webster] or Cool Path Duo [St. Jude Medical]) |
Pulmonary vein puncture (n=1) |
– |
– |
79±25 |
|
Lin et al. (2009)41 |
Japan |
Single |
60 |
NPAF |
49 |
83.3 |
55 |
NavX (with CFE software; St. Jude Medical Inc.) |
20/60 (33.3) |
AF restored to SR during ablation |
CFE mapping |
Irrigated-tip 4 mm ablation catheter (EPT; Boston Scientific Corporation), circular catheter recording (Spiral, AF Division; St. Jude Medical Inc.) |
Patient with cardiac tamponade (n=1) |
19 |
25 |
n/a |
|
Lo et al. (2009)42 |
Japan |
Single |
87 |
Perm AF |
53 |
82.8 |
54 |
NavX (St. Jude Medical) |
30 (34.5) |
Termination to SR |
CFAE mapping |
Irrigated-tip 3.5 mm ablation catheter (Chilli II™, EPT; Boston Scientific Corporation, San Jose, CA, USA) and catheter recording (Spiral, AF Division; St. Jude Medical) |
Pericardial effusion needing pericardiocentesis (n=1) |
21 |
21 |
n/a |
|
Matsuo et al. (2012)43 |
Japan |
Single |
40 |
Pers AF |
53.5 |
97.5 |
62.4 |
EnSite NavX (St. Jude Medical) |
13 (32.5) |
Termination to SR |
CFAE mapping |
16-polar tow site (6-polar for the right atrium and 10-polar mapping catheter [Inquiry Luma-Cath; St. Jude Medical]), 20-polar circumferential mapping catheter of 20, 25 or 30 mm in diameter (Inquiry Optima; St. Jude Medical or Lasso, Biosense Webster) and irrigated 3.5 mm tip ablation catheter (CoolPath™ Duo [St. Jude Medical] or ThermoCool NaviStar [Biosense Webster]) |
n/a |
19.7 |
20 |
n/a |
|
Nair et al. (2009)44 |
India |
Single |
21 |
Perm AF |
44 |
42.9 |
n/a |
NavX EnSite software, version 7, at St. Jude Medical |
18 (85.7) |
Organization of the atrial electrograms or conversion into an SR |
CFAE mapping and voltage maps |
2 mm irrigated tip ablation catheter (IBI Therapy Cool Path Ablation Catheter; Irvine Biomedicals, Irvine, CA) |
No complications |
9.8 |
23.1 |
n/a |
|
Nakahara et al. (2014) 45 |
Japan |
Single |
60 |
Pers AF |
63.1 |
83 |
59 |
NavX, with CFE software (St. Jude Medical, Inc.) |
19 (31.7) |
Termination of AF to SR directly or via one or more intermediate ATs |
CFAE mapping |
20-pole, 15–25 mm Lasso catheter with 6 mm bipole spacing (Biosense Webster), 4 mm irrigated-tip catheter (Safire; St. Jude Medical) and 20-pole, 20 mm AFocus II catheter with 4 mm bipole spacing; St. Jude Medical) |
n/a |
16 med |
21.7 |
44.8±8.1 |
|
Roux et al. (2009)46 |
USA |
Single |
22 |
Pers AF |
58 |
82 |
60 |
NavX system (NavX, St. Jude Medical) |
2 (9.1) |
AF termination with PVI |
CFΑE mapping |
Mapping catheter (10-pole, 15–25 mm Lasso, 6 mm bipole spacing; Biosense Webster) and an 8 or 3.5 mm irrigated-tip catheter (Biosense Webster) |
n/a |
n/a |
n/a |
99±35 |
|
Suenari et al. (2011)47 |
Taiwan |
Single |
23 |
PAF |
54.3 |
83 |
59 |
EnSite NavX (St. Jude Medical, Inc.) |
16/23 (69.6) |
Termination of AF to SR directly or through one or more intermediate ATs |
CFAE mapping |
Irrigated 3.5 mm tip ablation catheter (EPT; Boston Scientific Corporation), 7F 10-pole/6F 4-pole catheters (St. Jude Medical Inc.) and 5F 12-pole circular catheter (Spiral, AF Division; St. Jude Medical Inc.) |
n/a |
11.9 |
24 |
n/a |
|
Verma et al. (2011)48 |
US |
Single |
30 |
Pers AF |
63 |
75 |
52 |
EnSite NavX mapping system (St. Jude Medical) |
4 (13.3) 3 (10%) (termination to SR) |
AF termination to SR or AT |
CFAE mapping |
Circular mapping catheter with ten 2 mm electrodes and 2 mm interelectrode spacing (Lasso; Biosense Webster) and 3.5 mm tip ablation catheter (ThermoCool; Biosense Webster) |
Left femoral haematoma (n=1) |
12 |
43 |
55±20 |
|
Narita et al. (2010)49 |
Japan |
Single |
51 |
AT |
57 |
54.9 |
n/a |
EnSite Multielectrode array (version 3.2 in 33 patients; version 6.0J in 18 patients) |
99 |
AT termination to SR and subsequent non-inducibility |
Voltage and activation maps |
A 4 or an 8 mm tip steerable catheter (Fantasista [Japan Lifeline]; Blazer II [Boston Scientific]) |
No complications |
16 |
3.9 |
19±11 |
|
Patel et al. (2008)50 |
USA |
Single |
17 |
Post-AF ablation AT |
62 |
82.4 |
61 |
EnSite NavX |
96‡ |
AT termination to SR and non-inducibility |
Activation and entrainment |
3.5 mm-tip Celsius ThermoCool (Biosense Webster, Inc.) or Chili (Boston Scientific, Inc.), mapping catheter (Lasso or Optima catheters; Biosense Webster, Inc., and St Jude Medical, Inc.), PentaRay catheter is a 20-pole steerable mapping catheter arranged in five soft radiating spines (1 mm electrodes separated by 4, 4 and 4 mm interelectrode spacing) covering a diameter of 3.5 cm (PentaRay; Biosense Webster, Inc.) and irrigated ablation catheter |
No complications |
7 |
23.5 |
n/a |
|
Nagamoto et al. (2011)51 |
Japan |
Single |
33 |
Post-AF ablation AT |
59 |
n/a |
n/a |
EnSite version 6.0J (St. Jude Medical) |
24 (73) |
Termination of AT or change to another AT or non-inducibility |
CFAE ablation |
Livewire (St. Jude Medical), multielectrode array catheter (St Jude Medical), 20-pole circular electrode catheter (Optima; St. Jude Medical) and non-irrigated ablation catheter with an 8 mm tip (Fantasista; Japan Lifeline) |
Femoral arteriovenous fistula (n=1) |
21 |
9 |
n/a |
*Choo’s study provided separate data about the patient characteristics for CARTO and NavX mapping systems.
†Suleiman’s study provided data on AF, AFL and AT, while the baseline characteristics are provided only for the total population.
‡The denominators in these percentages are the total number of atrial arrhythmias and not the total number of the included patients.
§These are similar cohorts, and therefore, these data were used once in the quantitative synthesis.
AF = atrial fibrillation;AFL = atrial flutter;AT = atrial tachycardia;CFAE = complex fractionated atrial electrogram;EF = left ventricular ejection fraction;F = French;f/u = follow-up;Med = median;n/a = not available;NPAF = non-paroxysmal AF;PAF = paroxysmal AF;Perm AF = permanent AF;Pers AF = persistent AF;PV = pulmonary vein;PVAI = pulmonary vein isolation ablation;PVI = pulmonary vein isolation;SR = sinus rhythm.
Table 2: Baseline characteristics and main outcomes of the included studies related to ventricular arrhythmia catheter ablation procedures
|
Study (year) |
Country |
Single/multicentre |
N |
Mean age (years) |
Males (%) |
Clinical setting |
EF (%) |
Mapping system |
Mapping type |
Acute success/definition of success |
Complications (n) |
Catheter |
Follow up (months) |
Recurrence at follow up (%) |
Endo or epi or both |
Fluoroscopy time (min) mean±SD |
|
Ventricular tachycardia – PVCs |
||||||||||||||||
|
CARTO mapping system |
||||||||||||||||
|
Luther et al. (2016)52 |
UK |
Single |
15 |
68 med |
n/a |
Ischaemic CMP |
30 |
CARTO 3v4 (Biosense Webster, Diamond Bar, CA, USA) |
Ripple, voltage, point by point or using an automated point collection facility (ConfiDENSE Continuous mapping) |
85% (non-inducible in 2/15 at the beginning) |
None |
Μultielectrode PentaRay catheter; 3.5 mm tip SmartTouch ThermoCool catheter (Biosense Webster) |
6 med |
71 |
Endo |
n/a |
|
Marai et al. (2010)53 |
Israel |
Single |
11 |
71 |
100 |
Ischaemic CMP |
23 |
CARTO mapping and navigation system (Biosense Webster, Johnson & Johnson, USA) |
Pace and entrainment, activation, voltage and substrate |
82% (termination of clinical VT and/or non-inducibility) |
n/a |
Open-irrigated ablation catheter |
3 |
11.1 |
Endo |
n/a |
|
Volkmer et al. (2006)54 |
EU |
Single |
47 |
65 |
91.5 |
Ischaemic CMP |
30 |
CARTO |
Activation, voltage, substrate, entrainment and pace |
79.1% (non-inducibility of the clinical or any slower VT) |
n/a |
4 mm tip (NaviStar™) or a 3.5 mm irrigated tip electrode (NaviStar ThermoCool™; Biosense Webster Ltd), RefStar™; (Biosense Webster Ltd.) |
25.1 |
43.2 |
Endo |
23.7±19.2 |
|
Antz et al. (2007)55 |
EU |
Single |
69 |
66.2 |
88.4 |
Ischaemic CMP |
32.6 |
CARTO system (Biosense Webster, Inc.) |
Voltage, entrainment and pace |
90% (non-inducibility of the clinical or slower VT), 43 (63%) (non-inducibility of any VT) |
n/a |
Quadripolar 6F Josephson catheter (Biosense Webster, Inc.), decapolar 6F Parahis catheter (Biosense Webster, Inc.), 7F CARTO catheter, either non-irrigated (4 mm tip; NaviStar; Biosense Webster Ltd.) or irrigated (3.5 mm tip; NaviStar ThermoCool; Biosense Webster Ltd.) |
25 |
37.7 |
Endo |
24±13.5 |
|
Bogun et al. (2005)56 |
US |
Single |
23 |
68 |
n/a |
Ischaemic CMP |
21 |
CARTO, Biosense Webster Inc.) |
Voltage map |
74% of VTs (targeted VT was successfully ablated) |
n/a |
NaviStar catheter (Biosense Webster Inc.) |
n/a |
n/a |
Endo |
n/a |
|
Brunckhorst et al, (2004)57 |
US |
Single |
11 |
68 |
100 |
Ischaemic CMP |
24 |
CARTO (Biosense Cordis Webster) |
Voltage, pace and entrainment |
90.9% (successful ablation sites were localized within an isthmus identified by pace mapping) 45.5% (absence of inducible VT) 45.5% (absence of inducible clinical VT) |
n/a |
n/a |
n/a |
n/a |
Endo |
n/a |
|
Deneke et al. (2005)58 |
EU |
Single |
25 |
62 |
n/a |
Ischaemic CMP |
37 |
CARTOTM System (Biosense Webster®) |
Substrate map, voltage mapping and pace |
70% (no VT inducible) |
Patients without procedural success (epicardial origin-problematic access to the LV) (n=2) |
NaviStar DS catheter |
10 |
17.4 |
Endo |
n/a |
|
Dinov et al. (2012)59 |
EU |
Single |
102 |
67.7 |
86.3 |
Ischaemic CMP |
32 |
Niobe Stereotaxis magnetic navigation system (Stereotaxis Inc.), electroanatomical mapping system (CARTO-RMT; Biosense Webster, Inc.) or EnSite-NavX (St. Jude Medical Inc., St. Paul, MN, USA) |
Substrate and/or activation mapping entrainment pace |
96% (successful ablation of the clinical VT) 76.5% (successful ablation of all inducible monomorphic sustained VTs) |
Pseudoaneurysm (n=2), arteriovenous fistula (n=1), pericardial effusions (n=6) and liver injury (n=1) |
Irrigated-tip catheter (NaviStar ThermoCool; Biosense Webster Inc.) and irrigated-tip catheter (NaviStar ThermoCool-RMT; Biosense Webster Inc. or Trignum Flux Gold, Biotronik, Berlin, Germany) |
14 med |
26.9 |
Endo–epi in one patient |
n/a |
|
Kettering et al. (2010)60 |
EU |
Single |
7 |
66.6 |
n/a |
Ischaemic CMP |
32.1 |
CARTO system (Biosense Webster) |
Voltage and pace |
100% (elimination of all clinically documented or inducible VTs) |
No major complications |
6F quadripolar diagnostic catheter (Biosense Webster), irrigated-tip ablation catheter (NAVI-STAR, 7F, D- [or C-] type, 3.5 mm-tip; Biosense Webster) and 8 mm-tip ablation catheter (7F, mostly C-curve; Biosense Webster |
19 |
28.6 |
Endo |
n/a |
|
Li et al. (2006)61 |
EU and China |
Single |
14 |
65 |
92.9 |
Ischaemic CMP |
29 |
CARTO, NAVI-STAR (Cordis-Webster, Johnson and Johnson) |
Substrate, voltage, pace and entrainment |
78.6% (no VT inducibility) |
n/a |
NaviStar, ThermoCool (Cordis-Webster) |
7 |
21.4 |
Endo |
10±7 |
|
Jamil-Copley et al. (2015)62 |
EU |
Single |
21 |
69 |
95 |
Ischaemic CMP |
28 |
CARTO-3 (Biosense Webster Inc.) |
Voltage, LAT, entrainment, ripple |
19,1% (termination during ablation) 78% (non-inducibility) |
n/a |
5 mm NaviStar ThermoCool catheter (Biosense Webster Inc.) |
15.5 |
29 |
Endo |
n/a |
|
Verma et al (2005)63 |
USA |
Single |
46 |
65 |
89.1 |
Ischaemic CMP |
27 |
CARTO (Biosense Webster, Inc.) |
Activation, voltage and entrainment |
100% (identification of the successful ablation sites) |
Periprocedural stroke (n=1), femoral haematoma (n=1), femoral pseudoaneurysm (n=1) and prolonged hypotension (n=1) |
7F NaviStar (Biosense Webster, Inc.) |
17 med |
36.9 |
Endo–epi |
n/a |
|
Miyamoto et al. (2015)64 |
Japan |
Single |
11 |
59 |
24 |
Ischaemic, dilated CMP, sarcoidosis and HCM |
24 |
CARTO version 3 or XP |
Voltage, activation, entrainment and pace |
45.5% (VT termination and non-inducibility) |
n/a |
Open-irrigated tipped catheter, ThermoCool® (Biosense Webster, Johnson & Johnson) |
21 |
– |
Endo–epi |
n/a |
|
Yamashina et al. (2009)65* |
Japan |
Single |
72 |
43.6 |
44.4 |
Idiopathic RVOT |
n/a |
CARTO system (Biosense Webster) |
Activation, voltage and pace |
63 (87.5%) (absence of any spontaneous or induced clinical RVOT arrhythmias and no recurrence of any symptomatic ventricular arrhythmia) |
n/a |
7 F NaviStar (Biosense Webster) |
n/a |
n/a |
Endo |
n/a |
|
Suleiman et al. (2007)15 |
Israel |
Single |
15 |
59 |
49 |
RVOT VT |
n/a |
CARTO |
– |
12 (80) |
None |
|
33* refers to the total population |
26.7 |
– |
10.3* refers to the total population |
|
Parreira et al. (2013)66 |
EU |
Single |
32 |
43 |
25 |
Outflow tract VT |
n/a |
CARTO XP RMT (Biosense Webster) |
Pace mapping |
26 (81%) (first procedure) (suppression and non-inducibility of arrhythmia) |
None |
NaviStar RMT (Biosense Webster), NaviStar RMT ThermoCool (Biosense Webster) |
10.2 |
6.3 |
Endo |
10±7.8 |
|
Yamashina et al. (2010)67* |
Japan |
Single |
33 |
45.5 |
36.4 |
Outflow tract VT |
n/a |
CARTO (Biosense Webster) |
Activation and pace |
87.9% (absence of any spontaneous or induced clinical RVOT arrhythmias and no recurrence of any symptomatic ventricular arrhythmia) |
None |
NaviStar (Biosense Webster) catheter |
2 |
6.1% |
Endo |
n/a |
|
Tovia-Brodie et al. (2016)68 |
Israel |
Single |
18 |
60 |
66.7 |
Idiopathic (77.8%) and ischaemic VT (22.2%) (complete abolition of the clinical ventricular arrhythmia or non-inducibility of ischaemic ventricular tachycardia) |
48.6 |
CARTO Segmentation Module software (Biosense Webster) |
Activation, pace and substrate mapping |
Idiopathic: 78.6% and ischaemic: 100% |
None |
3.5 mm open-irrigated catheter (ThermoCool, SmartTouch; Biosense Webster) |
n/a |
n/a |
Endo and epi for ischaemic VT |
Ischaemic: 20.9±8.8 min and idiopathic: 22.95±12 min |
|
Verma et al. (2005)69 |
USA |
Single |
22 |
41 |
68 |
ARVC |
55 |
CARTO mapping system (Biosense Webster Inc.) |
Voltage and pace |
18 (82%) (non-inducibility of ablated VT or other sustained monomorphic VT) |
Cardiac tamponade (1) and femoral haematoma (2) |
7F 4 mm-tip deflectable ablation catheter (NaviStar; Biosense Webster Inc.) |
37 med |
36.4 |
Endo |
83±47 |
|
Satomi et al. (2006)70 |
Japan |
Single |
17 |
47 |
76.5 |
ARVC |
n/a |
CARTO |
Activation, voltage and pace |
88%† (no monomorphic VT was inducible) |
No major complications |
7F mapping/ablation catheter (NAVI-STAR; Cordis-Webstar, Johnson & Johnson) |
26 |
23.5 |
Endo |
n/a |
|
Rhythmia mapping system |
||||||||||||||||
|
Martin et al. (2019)71 |
EU |
Multicentre |
27 |
64.3 |
85.2 |
Ischaemic and dilated CMP |
36 |
Rhythmia |
Substrate, activation, entrainment and pace |
92.3% (non-inducibility) |
No complications |
Orion mapping catheter (Boston Scientific) |
51.6 |
18.5 |
Endo–epi |
44.4±12.4 |
|
Nührich et al. (2017)72 |
EU |
Single |
22 |
67 |
n/a |
Ischaemic and non-ischaemic, ARVC |
36 |
Rhythmia 3D electro-anatomical mapping system (Boston Scientific, Marlborough, MA, USA) |
Voltage and activation |
87% (non-inducibility) |
Tamponade (n=1) |
ThermoCool, D- or F-Type, 2–5–2 mm spacing (Biosense Webster) or Intella NAV OI; (Boston Scientific) |
4 |
10 |
Endo–epi |
20.7±1.6 |
|
Sultan et al. (2019)73 |
EU |
Single |
32 (VT 15 patients and VE 17 patients) |
63 |
90.6 |
Different clinical settings including ischaemic CMP and myocarditis |
47,2 |
IntellaMap Orion™ Mapping Catheter (Boston Scientific Corporation) in combination with the Rhythmia™ mapping system (Boston Scientific Corporation) |
Activation, pace, substrate and entrainment |
100% 9no inducibility) |
Femoral haematomas (n=3) |
Quadripolar diagnostic catheter (Inquiry™, 5 F, Fa.; Abbott), decapolar diagnostic catheter (Inquiry™, 6 F, Fa.; Abbott) |
6 |
20 |
Endo |
23.4±13.7 |
|
Viswanathan et al. (2016)74 |
EU |
Single |
19 (VT: 12 patients and VE: 7 patients) |
64 |
79 |
Ischaemic and non-ischaemic CMP, congenital HD, hypertrophic CMP and normal |
35 |
Rhythmia (Boston Scientific Inc.) |
Activation |
VE: 6/7 (86%) VT procedures: 8/13 (61.5%) complete success (non-inducibility) |
Femoral pseudoaneurysm (n=1) and groin haematoma (n=1) |
64-electrode mini-basket mapping catheter (IntellaMap Orion™; Boston Scientific Inc.) |
10 |
VT 25% VE: 14.3% |
Endo–epi |
41.8±17.5 |
|
NavX–EnSite–CardioInsight mapping systems |
||||||||||||||||
|
Lee et al. (2019)75 |
Taiwan |
Single |
28 (24 PVC and 4 VTs) |
48.8 |
42.9 |
RVOT PVCs or VT |
70 |
EnSite NavX or Velocity V5.0 3D mapping system (Abbott) |
Voltage, pace and activation |
78.6% (at least an 80% decrease in PVC burden by 24 h Holter ECGs 3 months later after ablation) |
1% pericardial effusion |
7F 4 mm quadripolar irrigated ablation catheter or a 7F 4 mm or 8 mm non-irrigated ablation catheter |
3 |
21.4 |
Endo |
n/a |
|
Nayyar et al. (2013)76 |
Australia |
Single |
22 |
67 |
95 |
Ischaemic CMP |
32 |
EnSite NavX (St. Jude Inc.) |
Entrainment and pace |
64%(no inducible VT after ablation, abolition of ≥1 clinical VTs with other VTs remaining inducible was considered a partial success and the inability to eliminate the clinical VT was considered as a failure) |
n/a |
3.5 mm tip irrigated ablation (CoolFlex [St. Jude] or ThermoCool [Biosense Webster]), 20-pole catheter (PentaRay; 2–6–2 mm interelectrode spacing) and 1 mm electrodes (Biosense Webster, Inc.) |
16 |
22.7 |
Endo |
n/a |
|
Miyamoto et al. (2010)77 |
Japan |
Single |
55 |
52 |
49% |
Organic heart disease: 7 patients and idiopathic VT: 48 patients |
n/a |
EnSite version 3.0 in 20 patients and version 6.0J in 35 patients |
Voltage, substrate, activation and entrainment |
95% (sustained VT was VT termination, subsequent non-inducibility of VT for focal VT and non-inducibility for non-sustained focal VT and PVC) |
No complications |
Quadripolar electrode catheter, 20-pole multielectrode catheters (St. Jude Medical, Minnetonka, MN, USA/Ten-Ten, St. Jude Medical) |
21 |
– |
Endo |
30±21 |
|
Nair et al. (2011)78 |
India |
Single |
15 |
44 |
80 |
ARVC |
n/a |
EnSite array mapping and non-contact electroanatomical mapping |
Activation, entrainment and pace |
86.7% (all of the inducible VTs were successfully mapped and ablated) |
No complications |
– |
25 |
13.3 |
Endo |
n/a |
|
Hocini et al. (2015)79 |
EU |
Multicentre |
24 |
45 |
58 |
Idiopathic PVCs and PVCs in the setting of HCM and ischaemic CMP |
58.4% |
3D mapping technique (ECVUE; CardioInsight Inc.) |
Activation |
100% |
None |
Quadripolar mapping catheter) and 4 mm tip ablation catheter (Biosense Webster) |
24.7 |
4.2 |
Endo |
8.8±1.5 |
*These were similar cohorts and, therefore, were included once in the quantitative synthesis.
†The percentage refers to the number of successfully ablated VTs.
ARVC = arrhythmogenic right ventricular cardiomyopathy;CMP = cardiomyopathy;EF = ejection fraction;endo = endocardial;Epi = epicardial;F = French;HCM = hypertrophic cardiomyopathy;med = median;n/a = not available;PVCs = premature ventricular complexes;RVOT = right ventricular outflow tachycardia; VE = ventricular ectopy;VT = ventricular tachycardia.
We excluded studies that did not report data about the acute success rates or the type of mapping system that was used for the ablation procedure. Furthermore, we excluded studies including only patients with congenital heart diseases, heart transplant recipients and children. Case reports/series, animal studies, studies on ventricular fibrillation ablation procedures and studies on hybrid ablation procedures have also been excluded.
Data extraction
The data extraction was performed independently by two authors (GB and KE). The following data were extracted: first author, year of publication, journal name, type of study (single or multicentre), type of arrhythmia (AF, AT, VT or PVCs), duration of follow-up, number of patients, gender, age, type of cardiomyopathy, left ventricular ejection fraction, type of mapping system, type of catheters, mapping techniques, acute success definition, acute procedural success rates, procedural complications, follow-up, arrhythmia recurrence during follow-up, fluoroscopy time and type of ablation (endocardial, epicardial or combined).
The quality assessment of the included studies was performed using the NIH Quality Assessment Tool.80
Results
Study search
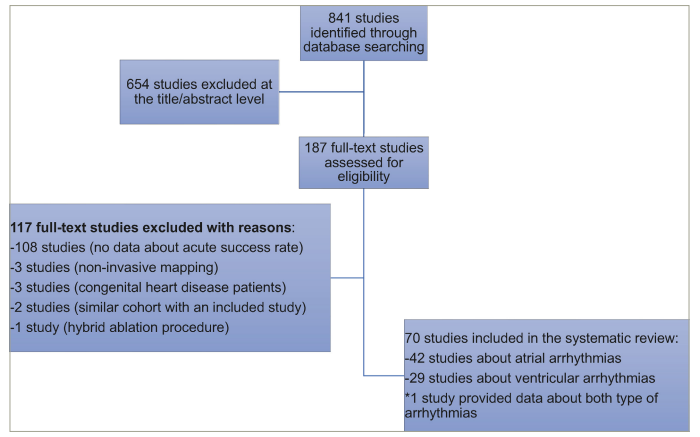
Of the 848 studies, 661 were excluded at the title/abstract level and 117 were excluded at the full-text level. Finally, 70 unique studies were included in the systematic review. Of them, 42 studies reported data about the acute procedural success of atrial CA procedures, while 29 studies provided data about the acute procedural success of ventricular CA procedures. One study provided data on both ventricular and atrial CA procedures.15 The search strategy is shown in Figure 1.
Figure 1: Flow diagram of the search strategy
Study characteristics
The baseline characteristics and the main findings of the included studies are presented in Tables 1 and 2 and in Figure 2.
Figure 2: Acute success rates and complications of commonly used mapping systems
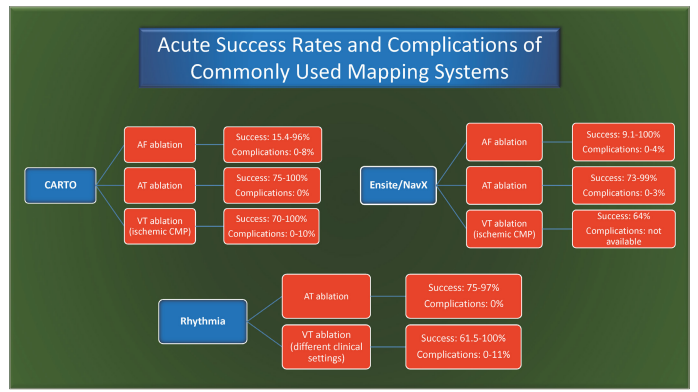
AF = atrial fibrillation; AT = atrial tachycardia; CMP = cardiomyopathy; VT = ventricular tachycardia
With regard to atrial arrhythmias, the search strategy revealed 17 unique studies that used the CARTO mapping system.11–26 Specifically, 10 studies provided data about AF ablation, 1 study on atrial flutter (AFL) ablation and 8 studies on AT ablation (one study provided data on all three types of arrhythmias).11–26 The Rhythmia mapping system was used in seven studies on atrial arrhythmias (two AF studies and five AT studies).27–33 Finally, in the setting of atrial arrhythmias, 20 studies provided data on the NavX/EnSite mapping systems (16 AF studies and 4 AT studies – 2 studies also provided data on the CARTO mapping system and therefore were included in both systems).12,20,34–51 As each of AF, AFL and AT has distinct electrophysiological mechanisms and substrates, we elected to report outcomes for each of these arrhythmias separately.
In the setting of ventricular CA, the search strategy revealed 20 studies that used the CARTO mapping system (12 studies in patients with ischaemic cardiomyopathy, 4 studies on outflow tract VT, 2 studies in the setting of arrhythmogenic right ventricular cardiomyopathy [ARVC] and 2 studies in mixed population); 4 studies that used the Rhythmia mapping system in mixed population including ischaemic and non-ischaemic cardiomyopathy, hypertrophic cardiomyopathy and congenital heart diseases and 5 studies that used the NavX/EnSite and CardioInsight mapping systems (one study in patients with ischaemic cardiomyopathy, one study in patients with ARVC, one study in patients with outflow tract VT and two studies in mixed population).15,52–69,71–79
All studies achieved a good quality rating according to the National Heart, Lung and Blood Institute study quality assessment tool (Online Supplement Table S1).81
Outcome data
Atrial arrhythmias
CARTO mapping system
In the clinical setting of persistent AF, CARTO exhibited a variable performance (10 studies) in terms of acute arrhythmia termination (Table 1). Specifically, in this setting, the acute success rates ranged from 15.4 to 96%, depending mainly on the type of AF and the definition of acute success (termination to sinus rhythm [SR] or termination of AF to any other organized rhythms).11–14,16–19,82
Furthermore, in the included studies, CARTO was used for the management of AT (eight studies). In this setting, the acute termination of ATs to SR ranged between 75 and 100%.20–26 Similarly, one study showed that the acute termination rate for AFL was 95% (Table 1).15
Rhythmia mapping system
Our search identified seven studies that used the Rhythmia mapping system for guiding CA procedures in patients with AT. These data showed excellent efficacy in terms of acute arrhythmia termination rates (Table 1).27–33
Furthermore, the search strategy revealed that the acute success rate for different types of AT (seven studies) ranged from 75 to 97%.28–33
NavX/EnSite mapping systems
In the setting of AF ablation, the use of the NavX/EnSite mapping system resulted in acute arrhythmia termination rates (16 studies), ranging between 9.1 and 100%, depending mainly on the type of AF (Table 1).12,34–48 However, it should be mentioned that the study that showed the lowest arrhythmia termination rate provided data about arrhythmia termination with PVI only in patients with persistent AF.46
The NavX mapping system was also found to have excellent efficacy in the setting of AT (three studies), with acute arrhythmia termination rates ranging between 73 and 99% (Table 1).49–51,83
Ventricular arrhythmias
CARTO mapping system
The CARTO mapping system has been used for the management of ventricular arrhythmias (20 studies) in different clinical settings (Table 2).15,52–70 The identified studies showed that the CARTO mapping system had an excellent efficacy in ischaemic cardiomyopathy (12 studies) CA ablation procedures.52–63 Specifically, the acute success rates are defined as the absence of VT inducibility at the end of the procedure, which ranged from 70 to 100%.52–63
Furthermore, the CARTO mapping system showed excellent results with more than 80% acute success rate in outflow tract ventricular arrhythmias and in the setting of ARVC (four and two studies, respectively).15,65–67,69,70
Rhythmia mapping system
The search strategy revealed four studies on the acute arrhythmia termination rates using the Rhythmia mapping system in the setting of ventricular arrhythmias (Table 2). These studies showed excellent results in abolishing VT and ventricular ectopy in different clinical settings, including ischaemic and non-ischaemic cardiomyopathy, with acute success rates ranging from 61.5 to 100%.71–74
EnSite/NavX mapping systems
The search strategy revealed five studies on the success rates of the EnSite/NavX mapping system, mainly in the setting of patients with outflow tract ventricular arrhythmias, ischaemic cardiomyopathy and ARVC (Table 2).75–79 Specifically, acute success rates were found to be 78.6% in patients with outflow tract arrhythmias, 86.7% in patients with ARVC and 64% in patients with ischaemic cardiomyopathy.75–79
Discussion
Our review summarizes the acute success rates of the most popular mapping systems across different clinical settings. The existing evidence shows that the most commonly used mapping systems have excellent efficacy regarding acute arrhythmia termination outcomes in both atrial and ventricular arrhythmias, depending mainly on the type of arrhythmia and the clinical setting.
Cardiac mapping is an essential component in the understanding and treatment of arrhythmias through CA procedures. Activation and electrocardiographic signal amplitude mapping are the most frequent modalities in 3D mapping systems, while entrainment mapping can provide additional data in the setting of atrial or ventricular arrhythmias. The commonly used 3D mapping systems such as CARTO (Biosense Webster), EnSite Precision (Abbott) and, more recently, Rhythmia (Boston Scientific) systems have played a major role in enabling and facilitating the high-density mapping of complex arrhythmias.3 The in vitro and in vivo accuracy of the CARTO mapping system has been studied since 1997.84 The CARTO mapping system has been used to guide the ablation procedure in patients with different types of atrial arrhythmias, including AF, AFL and AT.11–14,16–26,82
Today, the CARTO 3 system consists of a location pad with three separate low-level magnetic field-emitting coils arranged as a triangle under the patient’s body and six-electrode patches positioned on the patient’s back and chest. The latest version relies on hybrid magnetic- and current-based localization technologies and has reported an accuracy of less than 1 mm.3 On the other hand, the current EnSite/NavX navigation and visualization technology consists of a set of three pairs of skin patches and a system reference patch, and uses hybrid impedance-based and magnetic-tracking technologies to create cardiac models or geometries, which display voltage data and activation timing. The Rhythmia mapping system, which uses a hybrid tracking technology using both magnetic- and impedance-based localization features for map creation, was developed as a high-definition system incorporating a high-resolution 64-electrode catheter, 3D ultra-high-density mapping capabilities and an algorithm that automates the signal capture and mapping processes.3,85
Each of the mentioned systems, except NavX, uses its catheters for high-density mapping. CARTO 3 uses the PentaRay catheter and the Rhythmia system uses the IntellaMap Orion catheter, while the NavX system allows the operator to use any available catheter.
Single and multielectrode acquisition techniques are clinically effective, whereas a trend towards multielectrode use has been observed in the mapping of complex arrhythmias, such as left AFL and scar-related VT.86 A pooled analysis of studies that compared fluoroscopy- with non-fluoroscopy-guided ablation of AF and AFL showed that non-fluoroscopic mapping and navigational systems yielded acute success rates not significantly different from fluoroscopy-guided ablation, while navigational systems resulted in a 10% relative reduction in the overall failure rate compared with fluoroscopy-guided ablation for the treatment of AF.87 Another interesting finding was that mapping systems were shown to reduce the arrhythmia burden and the need for antiarrhythmic drugs in patients with complex arrhythmia following a failed fluoroscopy-guided ablation procedure.87
Few studies in the literature have performed direct comparisons of the most commonly used mapping systems. Specifically, Liu et al. performed a direct comparison of CARTO-guided with EnSite/NavX-guided ablation of the PV in AF.88 They found that compared with the CARTO group, the EnSite/NavX group had a significantly higher acute success rate. Specifically, AF was terminated by radiofrequency delivery in 14 cases (35%) using EnSite/NavX system versus 5 cases (14%) in the CARTO system (p<0.05).88 In addition, complete PV isolation was achieved in 26 cases (65%) in the EnSite/NavX group versus 11 cases (31%) in the CARTO group (p<0.05), although contemporary techniques and outcomes have resulted in much higher success rates.88 On the other hand, Choo et al. did not find a significant difference in acute success rates between CARTO and NavX mapping systems in the setting of paroxysmal or persistent AF CA.12 In another study, the acute outcomes of AT ablation using standard (CARTO™ and NavX™) versus Rhythmia™ 3D high-density mapping systems were compared; in this setting, acute success rates were found to be similar for any system, leading to around 75% complete and 93% partial acute success rates in a highly selected population.89 Rottner et al. performed a direct comparison of CARTO and Rhythmia mapping systems in the setting of AF.90 This study showed that the Rhythmia mapping system had a significantly longer total mapping time, a longer total fluoroscopy time, more delivered RF applications and a longer total RF duration compared with the CARTO system, while there was no difference regarding the total ablation time, total procedure duration and acute procedural success.90 Another study evaluated the effect of Rhythmia in terms of the outcome of the second ablation for AF compared with the conventional method with an additional anatomical guide by the CARTO system.91 The authors have found that high-density mapping for the second ablation of AF was superior to the conventional ablation method in terms of the suppression of atrial events.91 Kaseno et al. evaluated PentaRay®/CARTO® 3 and Orion™/Rhythmia™ in LA voltage mapping.92 The study showed that the PentaRay map had a shorter procedure time than the Orion map, while a discrepancy in the evaluation of low-voltage areas between PentaRay and Orion maps was revealed.92
Finally, it should also be noted that while acute AF termination has been a common goal of AF ablation, in more recent years, the focus is more on a substrate ablation strategy (PVI and often additional ablation), and now the acute completeness of PVI and long-term freedom from arrhythmias are more typical endpoints.5
Limitations
We identified only a small number of studies27–51 on acute arrhythmia termination during CA procedures for the Rhythmia and NavX/EnSite mapping systems, especially in the setting of ventricular arrhythmias. Specifically, no data were revealed by the search strategy about the acute success rates in AF CA procedures using the Rhythmia mapping system, while only one study (Nayyar et al.) provided data about ischaemic VT for the EnSite mapping system.76 Furthermore, no data on the CardioInsight mapping system were retrieved.
It should be noted that Rhythmia is a more recently developed mapping system compared with CARTO and EnSite; therefore, the studies on Rhythmia included in this analysis are likely to be more recent, compared with studies on CARTO and EnSite and, therefore, could skew the results.
A quantitative synthesis to estimate the pooled success rate of each mapping system was not performed. With regard to AF, beyond PVI, there is no single established strategy; as a result, differences in success rates are also dependent on the ablation strategy. Furthermore, the type of AF (paroxysmal, persistent and long-standing persistent AF) also influences the success rate of the ablation procedure. Similarly, AT ablation is largely dependent on the underlying arrhythmia mechanism, atrial substrate and ablation strategy. With regard to the ventricular arrhythmias, both the type of cardiomyopathy and ablation strategy can influence the ablation outcomes. Ablation for VT is often performed during SR using substrate modification of local abnormal ventricular activities due to the hemodynamic instability associated with the arrhythmia.93 Therefore, our results cannot be extrapolated to procedures using substrate modification for ventricular arrhythmias.
We chose not to provide data about the procedural time presented in each study because this parameter is dependent on not only the technical characteristics of each system but also the operator’s skills. In addition, this review did not focus on the long-term arrhythmia recurrence rate because this marker is highly dependent on patients’ comorbidities, post-procedural medications, echocardiographic findings, follow-up strategy for the identification of arrhythmia recurrence, etc. It should be noted that acute success definitions differ slightly among the included studies (Tables 1 and 2), and this is an additional limitation that prevents the comparison of the efficacy of the different mapping systems in all clinical settings. Another cause of the noted discrepancy in success rates for each mapping system among the included studies could be related to the new features that were incorporated into each system and the different catheters that were used in the last few years.
Conclusions
Mapping systems have played a crucial role in high-density mapping and the observed high procedural success rates of atrial and ventricular CA procedures. More data are needed about the comparative efficacy of the different mapping systems across different clinical settings.