Background: Right ventricular pacing (RVP) to reduce left ventricular outflow tract (LVOT) obstruction in hypertrophic obstructed cardiomyopathy (HOCM) remains controversial. Imprecise and variable atrioventricular delay (AVD) selection methods have contributed to the uncertainty. Using automated, high-precision AVD selection methods that target cardiac output incrementation may allow reliable identification of the optimal AVD to determine whether optimised RVP is beneficial in HOCM.
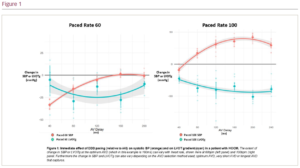
Methods: A total of 15 patients with HOCM and dual chamber pacing devices in situ were recruited. Pacing was alternated between atrial pacing (AAI) and AV sequential RVP (DDD) 10 times whilst beat-by-beat blood pressure (BP) via non-invasive finometry and LVOT continuous wave Doppler for LVOT gradient (LVOTg) via echocardiography were continuously recorded. This was repeated for a full range of AVDs at 10 bpm above sinus rate and 100 bpm. Custom software automated detection of LVOTg trace troughs and BP trace peaks to identify beat-by-beat LVOTg and systolic blood pressure (SBP), respectively. The mean difference in LVOTg and BP between pacing states (AAI and DDD) were plotted for each AVD and fitted to quadratic curves to improve precision (Figure 1). The peak of SBP curve identified the optimal AVD for cardiac output. Averaging changes in beat-by-beat SBP and LVOTg across multiple pacing transitions accounts for physiological drift and automated analysis reduces bias.
Results: Mean LVOTg of recruited patients was 50 mmHg at rest. At 10 bpm above sinus rate, DDD pacing at optimal AVD significantly increased SBP (+2.72 ± 1.33 mmHg; p=0.05) and significantly reduced LVOTg (-12.4 ± 3.64 mmHg; p=0.002). At 100 bpm, greater SBP increases were seen (+10.0 ± 3.96 mmHg; p=0.02) with greater LVOTg reductions (-23.7 ± 6.95 mmHg; p=0.004). Alternative described methods for AVD selection also reduced LVOTg but with worse SBP responses. Longest fully captured AVD reduced LVOTg (-3.34 ± 2.05 mmHg) but increased SBP by a smaller amount than optimal AVD (+1.36 ± 1.1 mmHg). Very short AVD (40–80 ms) reduced LVOTg (-5.55 ± 4.3 mmHg; p=0.2) but substantially reduced SBP (-23.5 ± 3.22 mmHg; p<0.01).
Conclusion: High precision, automated haemodynamic measurements detected the optimum AV delay that balanced the increased LVOT size, reduced myocardial performance and altered AV filling that occur with RVP for HOCM. AVD-optimised RVP reduced LVOTg and improved cardiac output. ❑