Bradycardia, renal failure, atrioventricular nodal blockade, shock and hyperkalemia (BRASH) syndrome is a rare, often unrecognized but potentially life-threatening clinical entity that is characterized by the pentad of symptoms after which it is named. BRASH syndrome is seen most commonly in the setting of atrioventricular nodal-blocking medications such as beta-blockers and calcium channel blockers.1,2
The synergistic interplay of low cardiac output state, renal function and high potassium creates a vicious cycle that can escalate quickly. Hyperkalemia can cause bradycardia, which can lead to low cardiac output and poor renal function. As the kidneys are unable to clear potassium from the bloodstream effectively, this can exacerbate hyperkalemia. Hyperkalemia in the setting of atrioventricular nodal-blocking agents can further impair electrical signalling in the heart, which can progress to cardiogenic shock, cardiac arrest and, ultimately, death.3
Given the potential consequences of BRASH syndrome, and its often rapid course, a thorough understanding of the underlying mechanisms and clinical context is necessary for improving patient outcomes and reducing the risk of associated serious adverse events. Across the literature, there remains a variety of clinical presentations, precipitating factors and treatment methods, indicating the need for further study.4
This case report represents an uncommon presentation of bradycardia, renal failure, atrioventricular nodal blockade, shock and persistent hyperkalemia that was refractory to conservative management, in the setting of digoxin toxicity.
Compliance with ethics
Ethics approval was not required for this case report, as it was deemed not to constitute research, by the Rutgers Institutional Review Board. This research was a retrospective chart review study and is not subject to institutional review board approval. The study was performed in accordance with the Helsinki Declaration of 1964, and its later amendments. Verbal consent was obtained from the patient for this case study by the primary medical team. The verbal consent was obtained by the primary medical team over the telephone after the patient was discharged to the rehabilitation facility. Due to the patient being at the facility, obtaining a written consent was deferred and the patient was assured that no patient identifying information would be used for any research reports. No identifying patient information is included in this manuscript.
Case presentation
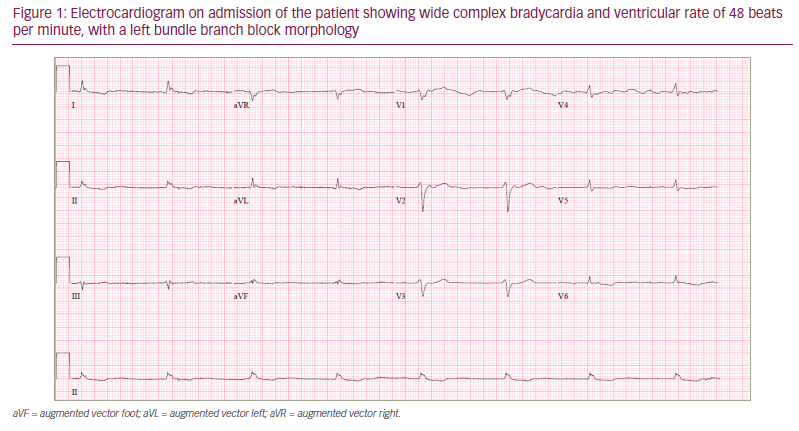
An 81-year-old male presented to an outpatient appointment with progressive dyspnoea on exertion, confusion and abdominal distention, all which began a few days prior to the appointment. He had a past medical history of hypertension, type 2 diabetes mellitus, heart failure with preserved ejection fraction (ejection fraction of 58%), atrial fibrillation on apixaban and digoxin, mitral regurgitation, tricuspid regurgitation, lung cancer, and right middle and lower lobectomy. At the doctor’s office, the patient was found to be bradycardic (25 beats per minute [bpm]) with a blood pressure of 85/38 mmHg. The doctor referred the patient to the emergency room, and en route, 1 mg of intravenous atropine was administered for bradycardia, resulting in an improvement of heart rate to 40 bpm. Laboratory results on arrival in the emergency department were notable for potassium level of 6.9 mMol/L, creatinine level of 3.10 (baseline 0.7), and digoxin level of 2.7 ng/mL. The electrocardiogram showed wide complex bradycardia and ventricular rate of 48 bpm, with a left bundle branch block morphology (Figure 1). The patient was given a 2 L fluid bolus and was started on dopamine drip for bradycardia and hypotension. For his hyperkalemia, he was treated with 1 g intravenous calcium gluconate, and 10 units of intravenous insulin and dextrose-50. In the setting of elevated digoxin levels and acute renal failure, digoxin was discontinued and 2 vials of digoxin antibody (DigiFab®; BTG International Inc., Conshohocken, PA, USA), 40 mg each, were administered to the patient. Subsequent laboratory results after the initial interventions showed that his potassium levels remained elevated at 6.7 mMol/L. A clinical decision was made to start continuous renal replacement therapy (CRRT) in the setting of acute renal failure. In the subsequent days, his blood pressure, bradycardia, and mentation progressively improved, and he was weaned from the dopamine drip. The patient was also weaned from the CRRT treatment after 4 days, and his kidneys appropriately responded to an intravenous furosemide challenge, with 2.5 L of urine output. On the sixth day after admission, the patient developed aspiration pneumonia, for which he was treated with 4.5 g of piperacillin-tazobactam intravenous antibiotics, every six hours for five days. Ten days after admission, he was eventually discharged to a subacute rehabilitation facility.
Discussion
Recognizing BRASH syndrome and differentiating it from isolated hyperkalemia-induced arrythmias is an important step in clinical decision-making, and management of a patient that presents with this clinical entity. Calcium channel blockers and beta-blockers have been recognized as pharmacologic agents associated with BRASH syndrome in the literature.5,6 However, digoxin-associated BRASH syndrome has not been widely reported. Management of this clinical entity can include interventions to correct any or all five of its symptoms. Initial stabilization with calcium gluconate, insulin/glucose, transvenous pacemaker, vasopressor medications, and haemodialysis are mainstay treatments reported in the literature.7–9 The patient in this case was initially treated with fluid resuscitation and dopamine to manage his shock. He was also simultaneously treated with insulin and glucose to correct hyperkalemia. Digoxin was withheld, as it contributed to the synergistic mechanism of BRASH syndrome, and digoxin antibody was administered to reverse the digoxin toxicity. Soon thereafter, a clinical decision was made to start CRRT in the patient, as his acute renal failure had not improved with the given interventions. The limitations of this case are that generalization of BRASH syndrome management cannot be made as it is patient-centered, and the treatment outlined here may vary from case to case as there are no consolidated treatment guidelines in the literature.
As seen in this patient, multiple medical interventions are required in a timely manner to stop the synergistic mechanism involved in BRASH syndrome. Since the decision for haemodialysis was concerning, due to shock, CRRT was pursued as an alternative to correct hyperkalemia and acute renal failure. This case demonstrates that early and aggressive interventions are lifesaving when there is a high index of suspicion for BRASH syndrome.