Background: A type 1 Brugada pattern (T1-BrS) is a recognised marker of arrhythmic risk. Twelve-lead 24-hour Holter monitoring with V1 and V2 in standard and high precordial electrocardiogram (ECG) lead (HPL) positions, can identify transient spontaneous T1-BrS pattern in BrS patients with a concealed T1-BrS at presentation.
Aim: To investigate the yield and prognostic value of 12-lead 24-hour Holter monitoring with additional high precordial ECG leads (HPL-Holter) in a large single-centre cohort of BrS patients.
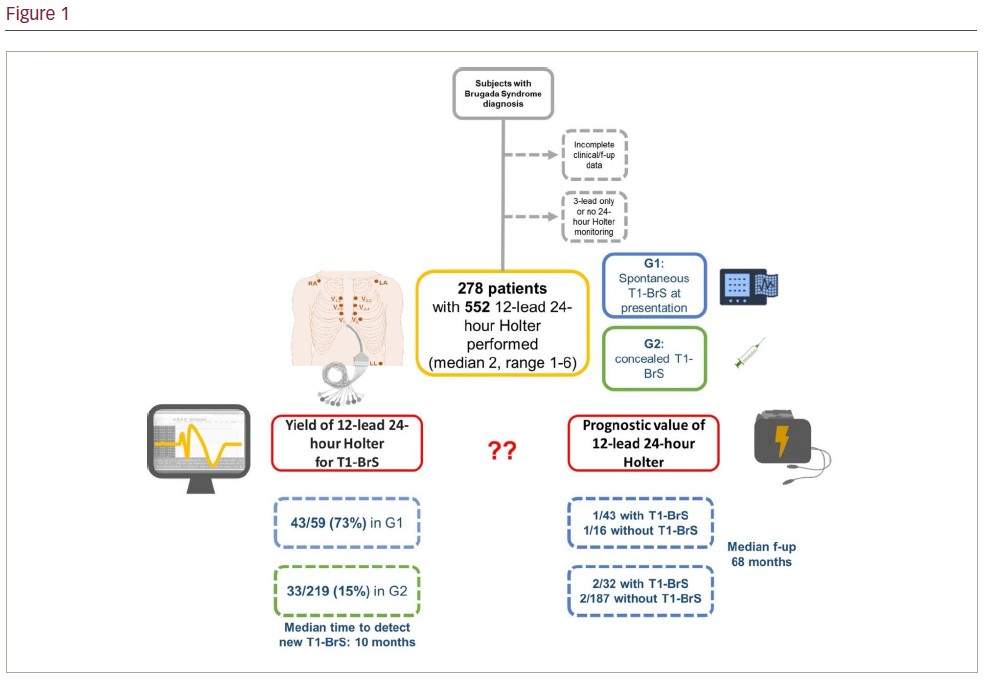
Methods: A total of 278 subjects with BrS (56% male, mean age at presentation 43 ± 15 years) were included in this study, for whom complete clinical and follow-up data and HPL-Holter(s) after initial evaluation were available. Of these, 59 had a spontaneous T1-BrS pattern at presentation (Group 1) and 219 did not (Group 2), usually requiring ajmaline provocation testing to confirm the diagnosis.
Results: From 2008 to 2022, 552 HPL-Holters were recorded in the study cohort (median 2, range 1–6). In total, 43 (73%) subjects in Group 1 and 32 (15%) in Group 2 showed a T1-BrS pattern during HPL-Holter monitoring at least once; this was evident on the 1st follow-up recording in 95% of cases in Group 1 and 66% in Group 2 (median 10 months, IQR 45, range 0.5–64), with at least 2 recordings needed in 28% of subjects in this latter group. Patients with a newly identified T1-BrS in Group 2 tended to be older (mean age 48 ± 14 vs 42 ± 16 years; p=0.05) and to carry the proband status (56% vs 52%; p<0.05) than those without, whereas there were no significant differences in gender, family history of sudden cardiac death and the presence of previous symptoms. Over a median follow-up of 68 months (IQR 64), significant arrhythmic events (appropriate ICD shocks on VT/VF) occurred in 2 subjects in Group 1 (1/43 showing T1-BrS during HPL-Holter monitoring and 1/16 not showing it; p=NS) and in 4 subjects in Group 2 (2/32 with newly identified spontaneous T1-BrS and 2/187 without; p<0.05).
Conclusions: Twelve-lead 24-hour ambulatory ECG monitoring including additional HPLs can identify a transient spontaneous T1-BrS in up to 15% of the subjects without the diagnostic pattern at presentation, most during the first year after the diagnosis. In this group, the presence of a T1-BrS pattern is associated with arrhythmic events. We recommend re-evaluation with high precordial 12-lead Holter monitoring of subjects without spontaneous T1-BrS at presentation once a year for at least the first 2 years post-diagnosis. ❑